https://photos.google.com/share/AF1QipMQvxwLXccd__GAPrMfLETFLypRyHzCHYlrEUlwOt-Dbw4Yhmhg8rzs85HJTBPLJA/photo/AF1QipOV8ip2fYhk3koRrfvsoNXM0N96-ZfJMVo40XDV?key=dGVweUZZaXZnV2Z6TDlFbGVDbXBkbjNzMnFUa1Z3
Archives: update
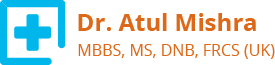
Pilonidal Sinus : Limberg Flap
????????? ????? : ??????? ????
A Pilonidal sinus is a small hole or tunnel in the skin. It may fill with fluid or pus causing the formation of a cyst or abscess. It occurs in the cleft at the top of buttocks (sacrococcygeal region). A Pilonidal sinus usually contains hair and debris. The name Pilonidal is taken from Latin meaning “???? ?? ?????”. It can cause severe pain or become infected. It may ooze pus or blood and have a foul odor. It mostly affects men and common in young adults. It is more common in people who sit for long time, like drivers.
??????
It is caused by a combination of changing hormones (puberty), excessive hair growth and friction from clothes or spending long time sitting.
Activities causing friction force the hair growing in the area to burrow back under the skin.
??? ?? ???????? ? ????????? ??????
There may be just a small dimple like depression on the surface of the skin of lower back in the natal cleft. It becomes symptomatic when infected.
The signs of infection include :
• Pain when sitting or standing
• Swelling of cyst
• Reddened or sore skin around the area
• Pus or blood draining from the abscess causing a foul odour
• Hair protruding from the lesion
• Formation of more than one sinus tract, or holes in the skin
????????? ????? ?? ???? ???????? ????? ?? ??????? ????:
• Excessive, coarse, curly or crinkly hair
• Deep natal cleft
• Poor hygiene
• Obesity
• Family predisposition
?????????
The most definite treatment for Pilonidal sinus is surgery.
If there is infection antibiotics can be given. This won’t heal the sinus-tract, but will give relief from the infection and discomfort.
It is recommended to regularly remove hair by clipping or shaving the site and maintain good hygiene.
???????
There are numerous procedures described to treat this condition. The most successful procedure with least recurrence is Limberg flap.
??????? ????
This technique involves wide excision of the area and closing a 60 degree rhombus-shaped defect with a transposition flap. This flap takes the suture line away from midline giving rise to tension free flap of unscarred skin in the midline, which helps in maintenance of wgood hygiene, reduced sweating, maceration, erosion and scar formation. It is superior to primary closure or other flap procedures and a safe & reliable method with low complication and recurrence rate.
?????????? ?? ??????? ????
• The patients get immense relief from the weeping and swollen bottom
• There is no distortion of the contour of the bottom
• This technique is easy to perform in quick time
• Very low complication rate and recurrence
• Quick healing time
• Short hospital stay
• Early return to work and daily activities
????????????? ??????????
Avoid pressure on flap for 3 weeks
??? ?? ??????? ????????? ??????
• Washing the area on a daily basis with a mild soap, making sure all soap is removed
• Keeping the area completely dry
• Avoid sitting continuously for long periods
??? ??? ????? ? ????? ?? ??????? ???? ????????? ?? ? ??????? ?? ????????? ????? ?? ????????? ?? ???? ??????? ?? ??? ??? ???? ???????
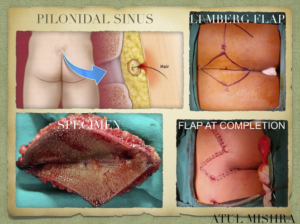
Appendicitis : Laparoscopic Appendicectomy
Appendicitis is an inflammation of the appendix, a finger shaped pouch that projects from colon (large intestine) on the lower right side of abdomen. The appendix does not have any specific purpose in our body. Appendicitis is the most common cause of abdominal pain resulting in surgery. More common in males and age group between 10 to 30 years.
????????
• Sudden pain on the right side of the lower abdomen.
• Pain that begins around navel and often shifts to lower right abdomen.
• Pain worsens by cough, walk or other jarring movements.
• Loss of appetite.
• Low grade fever.
• Constipation or diarrhea.
• Abdominal bloating
??????
A blockage in the lumen of appendix that results in infection leading to appendicitis. The bacteria multiply rapidly, causing the appendix to become inflamed, swollen and filled with pus. If not treated, the appendix can become gangrenous and rupture.
?????????????
• A ruptured appendix
Infection spreads throughout the abdomen requiring urgent surgery
• A pocket of pus
If localized burst of appendix occurs leading to development of pocket of infection (Appendicular abscess)
?????????
Blood test- High blood cell count
Urine test- To rule out urinary tract infection or kidney stone
Pregnancy test- To rule out ectopic pregnancy in female
Imaging test- Abdominal X-Ray, Ultrasound, CT scan
?????????
Mainstay of treatment of acute appendicitis is early surgery (within 24 to 48 hours).
Appendectomy is surgical removal of appendix.
???????????? ????????????
The surgery is done through few small incisions through which special surgical tools and a video camera are inserted into the abdomen to remove appendix.
?????????? ?? ???????????? ????????????
Early healing with less pain and scarring.
Faster recovery
???? ????? ??????? ??? ??????????? ????? ???????
• Avoid strenuous activity for 3-5 days
• Support your abdomen when you cough
• Children may return to school after a week
• Waiting period of 2-4 weeks to resume strenuous activity such as gym or sports
• There may be a temporary constipation. Staying hydrated and eating fiber rich food helps regulate bowel movement.
???????? ??? ???? ?? ???????????? ?? ???? ???? ?? ??????
• Fresh fruits and vegetables
• Kidney bean or other salads
• Swapping white rice for brown rice
• Using whole wheat flour
• Breakfast- cereals, yogurt and salads.
??? ??? ????? ? ????? ?? ???????????? ???????????? ???? ?? ?? ???? ?????? ?? ??? ??? ???? ???????
What you must know about varicose vein!
Varicose Veins is a condition in which an individual’s veins become swollen and warped or twisted, which is visible on the skin. This condition most often is prevalent in the legs but can occur in any part of the body. Varicose Veins is a common medical condition with a few symptoms and signs. It affects the skin tone and texture for which some people undergo a treatment.
These symptoms might not affect the person seriously, but they can get severe depending upon different conditions. Usually, Varicose Veins does not require medical treatment, but if it gets severe, then one needs to see the doctor or undergo surgery, which happens rarely. This condition can be easily diagnosed through physical examinations, but one might need to undergo some medical tests depending upon the severity of the condition.
Problems Related to Varicose Veins:
Some of the most common problems related to Varicose Veins are:
1. Telangiectasias: In this condition, blood vessels form a cluster, mostly on the upper body and face. They appear red and can be caused by many reasons such as genetic disarray, liver problems, pregnancy, or viral diseases. Although this is not something to worry about, one should consult the doctor if other symptoms accompany it too.
2. Spider Veins: This condition of Spider Veins is concerned with the smallest blood vessels called Capillaries. They are called spider veins because they develop mostly on legs and face and appear like a spider web. They are a moderate form of telangiectasias and hence does not really need medical treatment.
3. Varicoceles: Varicoceles appears in the scrotum region of the male body or over the testicle skin. This condition might result in infertility in males. A doctor should be immediately consulted if such a condition is seen.
Symptoms:
The Varicose Veins is not a serious medical problem unless the patient is going through severe pain and significantly manifested symptoms. There are many symptoms to identify the condition.
1. A visible cluster of blue or purple looking veins.
2. Frequent leg cramps.
3. Shrinking of skin of the ankle as a result of Lipodermatosclerosis (hardening of fat under the ankle skin).
4. Veins become tumefy or swollen and warped or twisted.
5. Ankles become swollen.
6. Throbbing legs.
7. Blood clots.
8. An unusual amount of bleeding in the affected part with a small injury.
9. Restless leg syndrome.
10. Scars like white, irregular patches on the ankle (Atrophie Blanche).
11. Redness, itchiness, and dryness on the affected area (stasis dermatitis or venous eczema).
12. Skin Discoloration.
13. Skin ulcers.
Precautions:
There are some precautions that one can take to relieve the pain caused by Varicose Veins.
1. Avoid standing for a longer period of time.
2. Maintain a healthy and balanced weight.
3. Sitting with legs straight and uncrossed.
4. Exercising.
5. Avoid wearing tight-fitting clothes.
6. Elevating legs while relaxing.
Take away:
Varicose Veins is a condition in which blood vessels get clustered in a part of the body under the skin. The veins appear blue or purple and become swollen and twisted. This condition is often not a serious medical problem, but in some cases, it might need surgery to avoid any serious issue. This can be treated by precautions and medications, but one can undergo surgery to get rid of the texture and view of the clustered veins. The recovery of Varicose Veins is quicker
Laparoscopic (Keyhole / Minimally invasive) surgery for cancer uterus
Total Laparoscopic Radical Hysterectomy (TLRH) – All About It!
Cervical cancer is one of the most common types of cancer in females. It is also one of the leading causes of death in women. Women in developed and developing countries, both are burdened alike from cervical cancer. Ineffective diagnosis, lack of awareness, neglect, ignorance, focus on other health issues, and insufficient attention to female health are the leading factors that are causing the graph to get steeper.
Cervical cancer can easily be detected in its early stages so that timely and appropriate treatment is possible. However, due to faulty and ill-equipped healthcare facilities, regular screening tests are not conducted. This leads to a delayed diagnosis and treatment, that aggravates the situation. Radical Hysterectomy is considered as the most important mode of treatment of cervical cancer. However, the clinical stage of cancer and its severity determine the plan of the treatment. It can either be only the surgery or a combination of surgery, chemotherapy and radiation depending upon the situation.
Total Laparoscopic Radical Hysterectomy (TLRH) is a minimally invasive procedure that shows promising results in the early treatment of cervical cancer. It is a safe and effective procedure. The procedure is associated with faster recovery, less loss of blood, faster return of bowel function post operation, fewer abdominal wall infections, better cosmetic result, and reduced febrile morbidity. Thus, it is preferred for Abdominal Hysterectomy. However, it consumes more time during the procedure itself.
Total Laparoscopic Hysterectomy includes detaching the entire uterine cervix from the body through laparoscopy and suturing the vaginal cuff with its surrounding supporting structures. The uterus is then removed through the abdomen or through the vagina.
When is it needed?
Total Laparoscopic Radical Hysterectomy is required when there is an evidence of cervical cancer. It is determined before the procedure by a biopsy done by the gynecologist. This surgery removes the primary source of cancer. It is also determined whether cancer has spread to any other or surrounding tissue.
Hence, a Radical Hysterectomy removes the uterus, cervix, and extra tissue around the cervix. If the cells in this tissue are non-cancerous, it is called ‘clear margins’ which is a good sign regarding the success of the surgery.
Before the Procedure:
A series of tests might be required to plan the surgery. These include blood profile tests, ultrasound, CT scans, MRIs, Echocardiography, Pulmonary Function Tests, etc.
Advantages:
• There are no large incisions in the abdomen because of the laparoscopic approach rather than the open surgery.
• There is less amount of blood loss during this type of surgery.
• There is less risk of infection.
• There is reduced febrile morbidity.
• There is less risk of adhesions. Adhesions refer to the sticking together of organs or tissues inside the body due to scarring.
• Bowel function returns to normal quickly in this case.
• There is less need for pain medication (analgesic) post-surgery.
• Shorter time is required to be spent staying at the hospital.
• There is a shorter recovery time involved and the patient is allowed to resume normal daily activities in a very short period of time, for example, generally within a month. However, heavy lifting should be avoided.
• There is an increase in patient comfort.
Take Away:
Total Laparoscopic Radical Hysterectomy (TLRH) is the most favored method for the treatment of cervical cancer in women. It is minimally invasive and easier to manage to post the procedure.
You can watch a video of Laparoscopic surgery for cancer uterus done by Dr Atul Mishra at our You Tube Channel :
Bowel Resection Surgery — Know Working Of It !
The bowel is a very important part of your body within the digestive system as it plays a vital role in the absorption of nutrients and minerals within your body as well as excreting toxic matter. The bowel contains the small bowel or small intestine as well as the large bowel or the large intestine. However, parts of the bowel may be infected or damaged in such a manner that they may need to be removed in order to save further worsening. Thus, the removal of sections of the bowels is known as bowel resection surgery.
How is bowel resection surgery performed?
In this procedure, sections of either the large intestine or the small intestine are removed which have either become diseased, infected or have malignant growths within them. The doctors and surgeons first identify the sections that need to be removed and then perform the surgery wherein a section of the tissue is excised and then two ends of the bowel are stitched together to form a new section of continuous small intestine or large intestine.
Types of bowel resection
There are two types of bowel resection, namely small bowel resection performed on the small intestine and large bowel resection performed on the large intestine. The indications for both of them are mentioned below:
Small Bowel resection:
Some of the cases wherein small bowel resection may be required are as follows:
• Cancerous or benign polyps or growth
• Precancerous growths and polyps
• Damage to the small intestine due to injuries
• Congenital defects in the small intestine
• Blockages in the intestine
• Growth of ulcers, bleeding, and infection within the small intestine
• Infections within the intestines
• Other disorders of the small intestine
Large bowel resection:
Large bowel resection is also carried out due to many of the same reasons as mentioned above. However, some of the specific reasons for large bowel resection are mentioned below:
• Colon cancer
• Diverticulitis, disorder that specifically affects the large intestine
• Bowel inflammation or ulcerative colitis
• Abnormal twisting of the bowel also known as volvulus
• Intestines which slide into another section of the intestine; also known as intussusception
Risks of the bowel resection
Like any other surgery, bowel resection also carries its own risks just as any other form of surgery. Some of the common risks of bowel resection are –
• Adverse reaction to anesthesia
• Infections
• Heart attacks or strokes during the operation
• Infections
• Excessive bleeding among others
Specific risks for large and small bowel resections are mentioned as follows:
•Small bowel resection:
Certain common risks include accumulation of pus in the abdomen, internal bleeding within the intestine after surgery, diarrhea, infection of the incision area and the stitched area breaking open among others
•Large bowel resection:
In this case, tissues protruding through the cut causing an incisional hernia is the most common element of risk. Nearby organs may be damaged as well; scar tissue, problems with the passage of material within the colon among others are some of the other complications.
However, these issues occur rarely and resections are performed very successfully and quite regularly by surgeons.
You can watch a video of Laparoscopic Intestinal surgery by Dr Atul Mishra at our You tube Channel:
Thyroid Surgery — Why Is It Required?
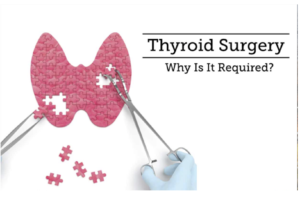
Thyroid is a small butterfly-shaped gland, which is present at the lower frontal region of the neck, right beneath the voice box. It produces hormones which regulate metabolism (the breakdown of food by the body to convert it into energy). It even plays a pivotal role in boosting organ functions as well as in helping the body to sustain heat.
However, too much of hormone production by the thyroid gland might yield structural problems, for instance, growth of nodules (abnormal tissue growth) or cysts (non-cancerous sac-like structures containing fluid) and swelling. Hence, thyroid surgery is a must once these problems occur. The surgery, administered with general anesthesia, eliminates the thyroid gland either wholly or partially.
Why do you need surgery?
1. The presence of tumors or nodules on one’s thyroid gland is one of the reasons why one should go for the surgery. Although most of the nodules are benign, few can be pre-cancerous or cancerous too. Also, those benign nodules can spell trouble, if they expand in size, thus obstructing the throat. They can be problematic as well if they cause the thyroid gland to overproduce hormones, giving rise to a condition known as hyperthyroidism.
2. Hyperthyroidism can be corrected through surgery. It is often an outcome of Grave’s disease, an autoimmune disorder wherein the body misidentifies the thyroid gland as a foreign body, thereby creating antibodies to combat it. The thyroid gland gets inflamed in the process, resulting in the overproduction of hormones.
3. Another reason is the enlargement or swelling up of the thyroid gland, termed as goitre. Similar to large nodules, goitre too can clog the throat, thus interfering with one’s breathing, speaking and eating.
Types of Surgery:
1. Lobectomy: This procedure calls for partial removal of the lobes when a nodule or an inflammation affects just half of the thyroid gland.
2. Subtotal Thyroidectomy: Here, a small proportion of the thyroid tissue is left behind even after the elimination of the thyroid gland.
3. Total Thyroidectomy: Through this procedure, the entire thyroid gland is taken out along with the thyroid tissue.
There are two main approaches to thyroidectomy:
• Conventional thyroidectomy involves making an incision in the center of your neck to directly access your thyroid gland.
• Endoscopic thyroidectomy uses smaller incisions in the neck. Surgical instruments and a small video camera are inserted through the incisions. The camera guides your surgeon through the procedure.
You Can watch a video of Endoscopic(Minimally invasive/Key hole) Parathyroid surgery by Dr Atul Mishra at our You Tube Channel:
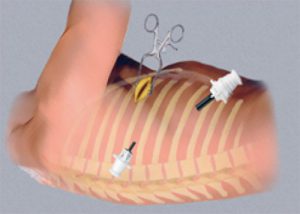
Laparoscopic Surgery — Know Why It Is Required!

There are many kinds of conditions and symptoms that require different kinds of surgery for treatment as well as diagnostic management. One such procedure is called laparoscopy or laparoscopic surgery. This is a surgical diagnostic management procedure that is known to be a low-risk process with minimal invasion and suitable for various types of ailments. Read on to know everything about laparoscopic surgeries.
•Definition:
A laparoscopic surgery is one where small incisions are made and an instrument called a laparoscope is used in order to take a look at the organs in the abdominal region. This tool is a long tube-shaped one that comes with its own high-intensity light and a high-resolution camera that can easily move along the walls of the organs while the camera sends back imagery that will be displayed on a video screen in front of the doctor. This avoids the need for open surgery and helps the doctors in getting samples for a biopsy on an outpatient basis.
•Need for Laparoscopy:
This procedure is performed when the patient complains of persistent pain that is also sharp and shooting, in the abdomen region and surrounding areas like the pelvic cavity. This non-invasive method helps in diagnosis where other imaging methods like an ultrasound and CT or MRI scans would have failed to give a conclusive reason for the pain and suffering of the patient. When these tests do not supply enough reason for proper diagnosis, then the doctors usually resort to this kind of procedure.
•The Organs it can be used for:
The laparoscopic surgery can be used for many organs including the appendix as well as the gall bladder, the pelvic region and the reproductive organs, the small and large intestines, the spleen, the stomach, the liver and the pancreas.
•What all can it Detect:
The laparoscopic surgery can help in detecting a number of issues including any abnormal growth or mass that may be a tumour. It can also point at the presence of any disease in the liver, as well as the proper functioning of certain treatments. Also, it can show the amount of fluid that may or may not be present in the abdominal cavity and the extent of cancer’s progression in the body.
Risks:
There are a few side effects or risks of this method including fever, chills, swelling, bleeding or redness of the site where the incision was made for the surgery, and shortness of breath. All these symptoms must be reported to the doctor immediately as they may point at the presence of an infection. Also, there is a risk of organ damage in this procedure.
You can watch a video of Laparoscopic Surgery for Cancer Rectum at our You Tube Channel :
VATS (Video Assisted Thoracic Surgery) — What Should You Know?
VATS (Video Assisted Thoracic Surgery):
The word surgery evokes fear in people’s hearts. This fear stems from the perception most people have of conventional surgeries, which include large incisions on the body and prolonged recovery times. However, today, due to the evolution of technology, some surgeries are minimally invasive. This means that not only is a large incision unnecessary in these surgeries but in some cases, the patient can walk out of the hospital on the same day as the procedure.
Video-assisted thoracic surgery or VATS is one such minimally invasive procedure, which helps diagnose and treat chest disorders.
What is VATS?
VATS is a type of minimally invasive surgery of chest. In this technique a small video camera called thoracoscope is inserted into the chest through a small cut to see inside and surgery is performed using special fine instrument through two or three small incisions (0.5 – 1cm). The thoracoscope transmits the image of inside of thoracic cavity onto a HD monitor. Other name of VATS are thoracoscopy, Thoracoscopic surgery or pleuroscopy.
Why is VATS done?
A number of reasons can prompt the doctor to prescribe VATS procedure for you. Here is a look at some common reasons –
• To conduct a biopsy for the diagnosis of mesothelioma, lung cancer & other cancers in the chest region, to identify infection or interstitial lung disease
• Surgery of the oesophagus
• To repair a hiatal hernia
• Surgery in the lungs for reducing lung volume or for lung cancer treatment
• To treat coughing of blood (Hemoptysis) due to fungal infection (Aspergilloma) or tuberculosis
• To conduct surgery for removal of excessive air or fluid from the region near the lungs
• To conduct surgery to prevent excessive sweating
• To remove the thymus gland
• To treat excessive GERD and acidity
• To treat hernia of Diaphragm or paralysis of diaphragm (eventration)
What are advantages of VATS?
In VATS, we make very small incisions causing very less trauma as compared to traditional “open” surgery. So, patient undergoing minimally invasive VATS procedure experience:
• Less pain after surgery
• Reduced bleeding during surgery
• Shorter operative time
• Reduced risk of infection after surgery
• Sorter hospital stay
• They recover more quickly and soon return to work (starting to earn their livelihood)
• Less incidence of long term (chronic) pain and shoulder dysfunction
• Better quality of life after VATS surgery
How to prepare for VATS?
Your doctor may ask you to undergo a few tests before the VATS procedure. These clinical tests help determine whether you are eligible for the surgery.
What to expect during VATS?
If you are undergoing VATS, it is likely that your doctor will administer general anaesthesia. You will be unconscious for the duration of the surgery. After administering the anaesthesia, the surgeon will insert a breathing tube through your throat. He/she will then make a small incision on your chest. Using specially designed instruments that contain a camera, he/she will perform the surgery.
After the procedure is complete, the surgeon will suture the area. Recovery from VATS: Due to the minimally invasive nature of the surgery, you will only need to stay at the hospital for a few days after the surgery. Post your discharge, you can go home and slowly get back to your daily life. However, you should let a family member or friend help you during this phase, because you may experience some pain from the surgery.
You can watch a video of VATS done by DR Atul Mishra at our You Tube Channel:
GALL BLADDER STONE: LAPAROSCOPIC CHOLECYSTECTOMY
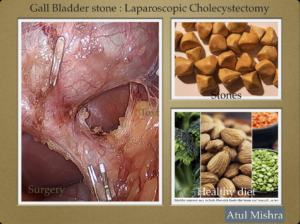
Gall bladder is a small organ below liver in the right side of upper abdomen. It is a pouch that stores bile, a green-yellow liquid that helps with digestion of fat.
Causes of stone formation:
80% of gall stones are made of cholesterol and 20% are made of calcium salts and bilirubin.
Having excess cholesterol in bile can lead to yellow, hard cholesterol stones. It may develop when liver makes more cholesterol than bile can dissolve.
Bilirubin is a chemical produced when liver destroys old red blood cells. Some conditions causing liver damage and certain blood disorders cause liver to produce more bilirubin. Pigment gall stones form when gall bladder can’t breakdown the excess bilirubin. These stones are dark brown or black.
Healthy and properly functioning gall bladder should empty bile regularly. If it fails to empty, the bile becomes over concentrated causing stone formation.
Symptoms:
Gall bladder stones can lead to pain in the upper right abdomen. Pain may start after intake of food high in fat, such as fried food. The pain usually lasts for a few hours.
It can also cause-
Nausea
Vomiting
Dark Urine
Clay colored stool
Stomach pain
Burping
Indigestion
Complications
Acute Cholecystitis
When a gallstone blocks the duct where bile moves from the gall bladder, it can cause inflammation and infection in the gall bladder.
Symptoms are: Intense pain in the upper stomach or mid-right back, fever, chills, appetite loss, nausea and vomiting.
Urgent medical consultation should be sought if symptoms last more than 1 to 2 hours.
Other complications:
Jaundice- Yellowish tint of skin or eyes
Cholangitis- Bile duct infection
Sepsis- blood infection
Pancreas inflammation
Gall bladder cancer
Risk factors for Gall Stones
Lifestyle
• Overweight (Obese)
• Eating diet high in fat or cholesterol, low in fiber
• Having rapid weight loss in a short period of time
• Diabetes Mellitus
Uncontrollable risk factors
• Female sex
• Family history of gall stone
• Age more than 60 years
Medical risk factors
• Cirrhosis of liver
• Pregnancy
• Medication for lowering cholesterol
• Medication high in estrogen content
Diagnostic Tests
Ultrasound
Abdominal CT scan
Gall Bladder Radionuclide Scan
Endoscopic Retrograde Cholangio Pancreatography (ERCP)
It is a procedure that uses camera and X-rays to look at the problems in the bile and pancreatic duct. It helps to remove gallstones stuck in bile duct.
Treatment
If gallstone is causing pain or other symptoms, surgery is recommended.
Laparoscopic Cholecystectomy
Surgical removal of gall bladder by minimally invasive key hole technique.
After gall bladder removal one may experience loose or watery stools. Removing the gall bladder involves rerouting the bile from the liver to small intestine. Bile no longer goes through the gall bladder and it becomes less concentrated. The result is a laxative effect that causes diarrhea. To treat this, a diet low in fat and high in fiber should be taken.
TIPS FOR HEALTHY GALL BLADDER
Life style changes in a patient having gallstone
• Maintain a healthy weight
• Avoid rapid weight loss
• Eat anti-inflammatory diet (Bell pepper, citrus fruits, green leafy vegetables, tomatoes, milk, fish, beans, nuts, lentils)
• Regular exercise
• Supplements – Vitamin C, Iron, Lecthin
Foods to avoid to reduce risk of gallstone
• Avoid high fat, greasy and fried foods
• Add fiber to your diet
• Avoid caffeinated drink, high-fat dairy produce and very sweet food
• Eat several small meals per day
• Drink sufficient amount of water (8-10 glasses /day)
You can watch a video of Laparoscopic Cholecystectomy for Gall Bladder stone done by Dr Atul Mishra on our You Tube Channel: